Regardless of the patho-anatomical etiology, most shoulder injuries involve a disruption in the delicate subacromial space (SAS). Once this space is altered the structures (joint capsule, articular cartilage, rotator cuff, biceps tendon, bursa) have increased risk for damage and misuse. This also leads to subsequent changes in muscle length-tension relationships, arthrokinematics, and motor patterns.The subacromial space is only 10mm. This is a very small amount of space to deal with; there is little room for error. To put this in perspective keep in mind that a dime is a little over 1mm thick. So even a very small change in the SAS could lead to potential clinical improvements. This increase in space will allow for decreased compression on structures and increased blood flow to allow for healing.Managing this space is very important in expediting the recovery process, especially in the acute phase. While assessing for movement dysfunction and physical impairments is important to develop an individualized plan of care, increasing the subacromial space will afford your patient decreased pain and increased function.
6 Ways to Increase Subacromial Space
- 1) Glenohumeral Adduction Force
- 2) Scapula Retraction, Upward Rotation, & Posterior Tilt
- 3) Increase Serratus Anterior Activation/Strength
- 4) Thoracic Extension
- 5) Good Posture & the Kinetic Chain
- 6) Rotator Cuff Co-Activation
Mechanism of Increasing Subacromial Space
1) Glenohumeral Adduction Force
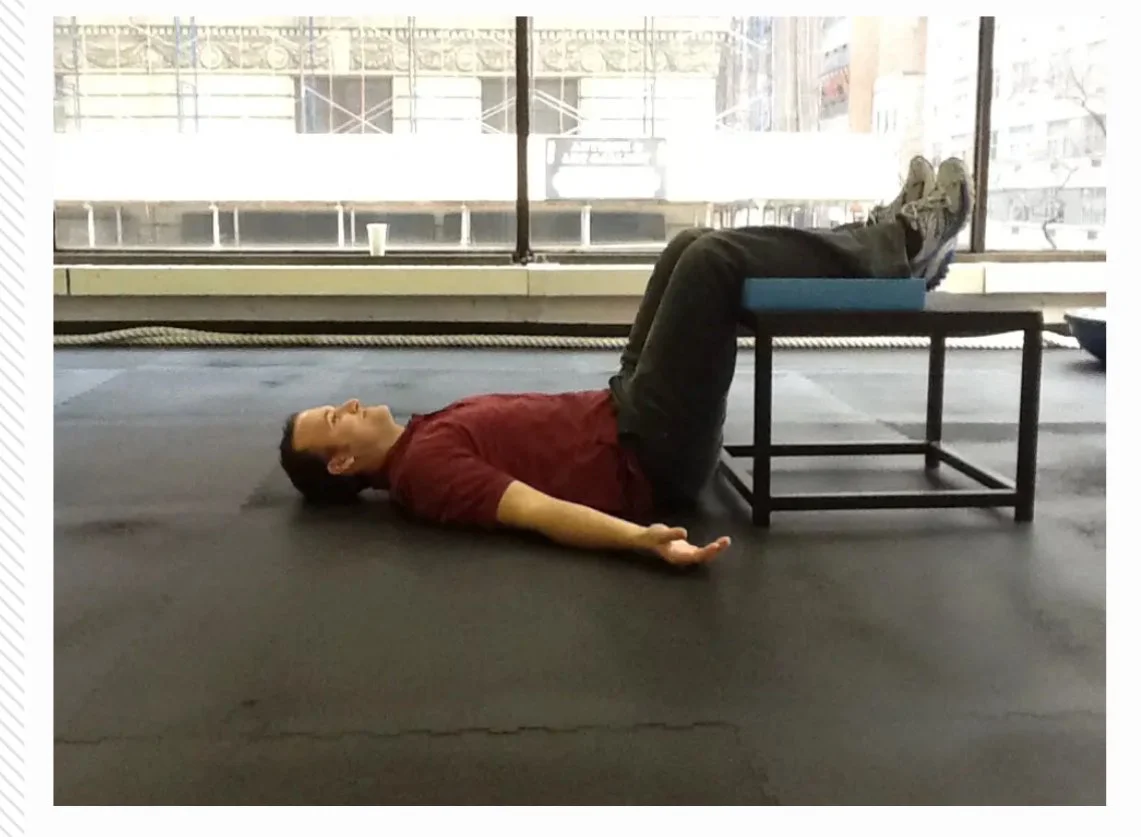
Most impingement tests involve a provocative glenohumeral abduction moment to decrease the SAS. So it would only make logical sense that glenohumeral adduction would increase SAS. Research has agreed with this logic and shown an shown that adducting muscle forces lead to a significant increase of the subacromial space (138% at 90 degrees relative to abduction forces). This adduction force can be used for everything from muscle energy techniques to simply holding a towel between your arm and torso. The latter can have a great effect during the acute stage and ensure reciprocal inhibition of the deltoid to decrease its superior compressive force on the SAS.
2) Scapula Retraction, Upward Rotation, & Posterior Tilt
Clinically I find the scapula to have the greatest impact on patients with impingement. A small alteration in the scapular orientation can greatly affect the amount of SAS. There is an overwhelming amount of evidence displaying altered scapula kinematics in patients with SAIS. More specifically, many studies have shown that scapula retraction, upward rotation, and posterior tilt increase the SAS. One study found that scapula retraction increases SAS by 200%. Most of these studies examine the kinematic differences between patients with impingement and pain free individuals. Here is what these studies have found in patients with SAIS:
- Decreased Upward Rotation (significantly at the end of the 1st of 3 phases - with concurent decreased UT firing)
- Increased Anterior Tipping at the end of the 3rd phase
- Increased Scapular Medial rotation under loaded conditions
There is an abundance of corrective exercises for the shoulder (just search on youtube). To emphasis an increase in SAS you should try to select exercises that strengthen/activate the muscles that produce scapula retraction, upward rotation, and posterior tilt.
3) Increase Serratus Anterior Activation/Strength
The serratus anterior gets its own section because of the unique role it has in controlling the inferior angle of the scapula against the thorax. This feature helps lift the anterior acromion off of the most common site of impingement. If you consider the scapula motionts that increase SAS you will notice that the serratus anterior has a role in each of these motions. Ludwig and Cook found that subjects with SAIS demonstrated decreased activity in this muscle across all loads and planes.
4) Thoracic Extension
Thoracic extension is an important part of the kinetic chain. It significantly alters scapular kinematics and is associated with decreased muscle force. Looking at the position of the thoracic spine will often display a correlated scapula position. For example, in the kyphotic thoracic spine the scapula would be anteriorly and superiorly tilted.We often consider treating patellafemoral patients by correcting the alignment and movement of the structures underneath the patella (dynamic valgus - femur & tibia). You can use the same logic to treat shoulder patients. Tom Myers has described the scapula as a sesamoid bone. Using this theory you could affect the scapula orientation and shoulder muscle forces by simply correcting the thoracic spine dysfunction.
5) Good Posture & the Kinetic Chain
While local interventions may have the most immediate impact, it is worth considering the global view of increasing SAS. Proper scapula position and thoracic extension are aspects of good posture, but in severe cases it is important to look at the bigger picture and modify posture from all angles. Research has shown that normal motor patterns of voluntary upper extremity movement include preparatory lower extremity and trunk muscle activation. Poor posture may alter optimal muscle length-tension relationships and effect the shoulder. It could be helpful to integrate a kinetic chain approach to accelerate rehabilitation and restore normal motor patterns.
6) RTC Activation
This is classic physical therapy and the conventional local method for increasing SAS. The rotator cuff externally rotates the greater tubercle away from the acromion and creates a concave compressive force. Studies have shown that there is reduced co-activation of the rotator cuff in patients with SAIS during the initiation of elevation below 30°, but not at higher angles. This validates the importance of reactive neuro-muscular training for the rotator cuff.
Bottom Line
This post was focused on the mechanisms and kinesiology that affects subacromial space. A full assessment is imparitive for effective treatment. By understanding the mechanisms that maximize the subacromial space you will have a better idea of what to look for and how to correct it.
6 Ways to Increase Space
- Glenohumeral Adduction Force
- Scapula Retraction, Upward Rotation, & Posterior Tilt
- Increase Serratus Anterior Activation/Strength
- Thoracic Extension
- Good Posture & the Kinetic Chain
- Rotator Cuff Co-Activation
References
Hinterwimmer, Stefan, Ruediger Von Eisenhart-Rothe, Markus Siebert, Reinhard Putz, Felix Eckstein, Thomas Vogl, and Heiko Graichen. "Influence of Adducting and Abducting Muscle Forces on the Subacromial Space Width." Medicine & Science in Sports & Exercise 35.12 (2003): 2055-059Solem-Bertoft E, Thuomas K-A¨ , Westerberg C-E. The influence of scapula retraction and protraction on the width of the subacromial space: an MRI study. Clin Orthop 1993;296:99-103Ludewig PM, Cook TM. Alterations in shoulder kinematics andassociated muscle activity in people with symptoms of shoulder impingement. Phys Ther 2000;80:276-91 (Best Article)McClure PW, Michener LA, Karduna AR. Shoulder function and 3-dimensional scapular kinematics in people with and without shoulder impingement syndrome. Phys Ther 2006 August;86(8):1075-90.Kebaetse, M. "Thoracic Position Effect on Shoulder Range of Motion, Strength, and Three-dimensional Scapular Kinematics." Archives of Physical Medicine and Rehabilitation 80.8 (1999): 945-50.Finley, M., and R. Lee. "Effect of Sitting Posture on 3-dimensional Scapular Kinematics Measured by Skin-mounted Electromagnetic Tracking Sensors☆." Archives of Physical Medicine and Rehabilitation 84.4 (2003): 563-68Myers JB, Hwang JH, Pasquale MR, Blackburn JT, Lephart SM. Rotator cu� coactivation ratios in participants with subacromial impingement syndrome. J Sci Med Sport. 2009;12:603-608McMullen J, Uhl TL. A Kinetic Chain Approach for Shoulder Rehabilitation. J Athl Train. 2000 Jul-Sep; 35(3): 329–337.Cordo PJ, Nashner LM. Properties of postural adjustments associated with rapid arm movements. J Neurophysiol. 1982;47:287–308 --The main reason I do this blog is to share knowledge and to help people become better clinicians/coaches. I want our profession to grow and for our patients to have better outcomes. Regardless of your specific title (PT, Chiro, Trainer, Coach, etc.), we all have the same goal of trying to empower people to fix their problems through movement. I hope the content of this website helps you in doing so.If you enjoyed it and found it helpful, please share it with your peers. And if you are feeling generous, please make a donation to help me run this website. Any amount you can afford is greatly appreciated.
[subscribe2]
 1) The popliteus is an important structure of the knee that is often overlooked by many clinicians. While it may not be the main contributor to knee dysfunction, it can still have a major impact. Some patients need greater activation of this muscle, while othersbenefit from a release. This is a good post on the popliteus and it's functional role in the knee joint.2) I recently had a patient with hamstring syndrome. She had been previously mis-diagnosed with piriformis syndrome, ischogluteal bursitis, lumbar radiculopathy, and hamstring tendonosis. Understanding how to differentially diagnose these patients may lead to a more specific treatment and a better outcome.3) Bret Contreas has a great post on Gray Cook. It's hilariously titled, "50 Shades of Gray Cook". I've been reading alot of Gray Cooks stuff lately. The more I read it the more I begin to think he is one of the most important figures in the future advancements of human movement. It's very innovative and complex without being very complicated. Which is difficult to accomplish in anything.4) Chris Johnson wrote a great post on calf strains ("tennis leg"). Very useful information on the acute management of this injury.5) I like the idea of bridging the gap between post-rehab and personal training. I think it would help rehab professionals to have a better understanding of training and the fitness industry. Pavel Tsatsouline is a very outspoken fitness guru. He has some great thoughts and opinions on training. I personally like his idea of "greasing the groove" and anti-muscle-failure approach. Chris Beardsly put it all in one place with his post of the top 10 Pavel Tsatsouline articles.
1) The popliteus is an important structure of the knee that is often overlooked by many clinicians. While it may not be the main contributor to knee dysfunction, it can still have a major impact. Some patients need greater activation of this muscle, while othersbenefit from a release. This is a good post on the popliteus and it's functional role in the knee joint.2) I recently had a patient with hamstring syndrome. She had been previously mis-diagnosed with piriformis syndrome, ischogluteal bursitis, lumbar radiculopathy, and hamstring tendonosis. Understanding how to differentially diagnose these patients may lead to a more specific treatment and a better outcome.3) Bret Contreas has a great post on Gray Cook. It's hilariously titled, "50 Shades of Gray Cook". I've been reading alot of Gray Cooks stuff lately. The more I read it the more I begin to think he is one of the most important figures in the future advancements of human movement. It's very innovative and complex without being very complicated. Which is difficult to accomplish in anything.4) Chris Johnson wrote a great post on calf strains ("tennis leg"). Very useful information on the acute management of this injury.5) I like the idea of bridging the gap between post-rehab and personal training. I think it would help rehab professionals to have a better understanding of training and the fitness industry. Pavel Tsatsouline is a very outspoken fitness guru. He has some great thoughts and opinions on training. I personally like his idea of "greasing the groove" and anti-muscle-failure approach. Chris Beardsly put it all in one place with his post of the top 10 Pavel Tsatsouline articles.